If you Google “brochure” and “family planning,” you get page after page of links to brochures, most of them to reputable materials you can use. But replace “family planning” with “Ebola,” and there aren’t so many options.
The outbreak, and our response, is simply too new. If you are in need of a brochure (or poster or radio spot or whole communication strategy) for Ebola – and you need it now, of course – you are going to have to build one. Luckily, you won’t have to do it from scratch.
There are communication materials for Ebola, and the Ebola Communication Network is making sure that they are being shared. But even if you find something that you think might meet your communication needs, you still are going to have to adapt it. Why? Because communication materials work best when they are specifically designed with an audience, topic and action in mind.
 For example, this nice poster was developed by the Ministry of Health and Social Welfare (MOHSW) and UNICEF in Liberia. Let’s say you want to use it somewhere else. Would it work? Could you just change the hotline number and the country logo and order a print run? Here are some things to consider before you do.
For example, this nice poster was developed by the Ministry of Health and Social Welfare (MOHSW) and UNICEF in Liberia. Let’s say you want to use it somewhere else. Would it work? Could you just change the hotline number and the country logo and order a print run? Here are some things to consider before you do.
1. What is my goal? What do I want people to know and do?
These are the first questions to ask. If the material doesn’t clearly and directly address the knowledge, behaviors or beliefs that you want to change, you are going to have to do an adaptation. This poster, for example, would be appropriate if your goal is for people to know the symptoms, call for help when they are sick and allow care by health care workers. This poster is appropriate in an active epidemic context where people have access to Ebola Treatment Units. But if you are working in a context where there are currently no Ebola cases but the community needs to prepare for a possible epidemic, the messaging will change to awareness of the signs and symptoms, rather than seeking care. In other words, your communication goal is going to be different in different places, and it will need to change over time as the situation changes, and your materials will need to change as well.
2. Is it right for my audience?
On a very basic level, you need to be sure that the people you are trying to reach can access and understand the information. If you are trying to reach poor women in an urban slum, because they are the family caregivers, you’ll need to be careful that the material is appropriate for a low literacy audience, and that the materials appeal to and catch the eye of the people who need to see it. So first define your audience, and then make sure the material is accessible and understandable to them. Two areas in particular are important when adapting for specific audiences:
Language: People are most likely to absorb the message of a material if the language is the language spoken in their home and community. Even if someone can speak English (or French, or what have you), the material might be more effective in a native tongue, especially if the material contains information that is influenced by culture. That creates a trade off: translating into multiple local languages and creating distribution plans for different sets of materials is more expensive and more time consuming than producing material in one language, and having one plan for its dissemination. But a material that isn’t understood or is ignored because it is perceived as coming from outside the community isn’t going to work, and that is an even bigger waste of time and money.
Images: Like language, pictures matter. If the material has graphics of people, houses, food, etc. they should look like the people, houses and food of the community for which the material is designed. Sometimes the graphics are simple enough that specific cultural or geographic cues aren’t noticeable, but often they are vitally important and getting it wrong can cause offense.
3. Is the information correct for my context?
Information that is correct in one context may be dead wrong in another. Carefully review the material to make sure that the information lines up with what local authorities are advising. Make sure hotline numbers, addresses and names of service providers are locally adapted.
4. Does the material have key messages?
Even if the information is generally what you want to communicate, materials are most effective when they have a few key messages. The Liberia poster is a good example of focus on a few key messages: the symptoms of Ebola and the steps to take if you have it. Sometimes communication materials can get too wordy or have too much information to absorb. Stick to a few key messages and if there is more information that is essential to communicate, put it on another material and distribute as companion pieces or try a different format.
There are many situations where a print material (or a radio PSA, or other short form mass communication) isn’t the appropriate way to communicate information. Complicated, in-depth information or information that contradicts cultural norms is best conveyed inter-personally or using video. This allows for back-and-forth communication with a trusted source (in the case of interpersonal communication) or at least modeling of behavior (in the case of a video). An example of complicated information would be how to care for sick family members at home while waiting for help. The instruction is best done by community health workers, while a print material or PSA could be used to encourage people to talk to those workers to get more information.
A sub-category of the key message is the “call to action,” which is the behavior you want people to take as a result of exposure to your material. This should never be ambiguous to you or your audience. Examples might be: “if someone in your family has a fever, call for care” or “protect yourself and your family, don’t touch dead bodies.” You should test the exact language of your call to action with the community to be sure you get it right.
So, say you have found a material that seems very close to what you need for your intervention. You have determined that it is appropriate for your audience, translated it into a few local languages and adjusted the language so it has a few key messages and a call to action that fits your context. Can you send it to the print house? Nope, not yet. One last important step.
5. Pre-test.
Before you invest time and money in producing materials, you need to be sure the audience understands them and reacts to them the way you intend. A pre-test doesn’t need to be formal or conducted by researchers. Here is a guide to conducting pretesting. When it comes to pretesting, do what you can do. Don’t decide to do none at all because you can’t do it the way the book tells you to. Any feedback is better than none.
Finally, a plea. If you are developing Ebola communication materials, or adapting existing materials, please share them with the Ebola Communication Network so others can adapt them all over again.
Ebola is Real: Using Theory to Develop Messaging in a Health Crisis
/in Social and Behavior Change Communication /by Lisa CobbQuestion: What is the difference between these two messages?
“Ebola is real! If you get it, you’ll die!”
and
“Ebola is real! If you seek treatment you have a fifty-per-cent chance of recovery?”
Answer: Theory. The Extended Parallel Process Model, or EPPM, to be exact.
These messages come from a great article in the New Yorker on the use of “culture makers” (i.e. entertainers, community leaders) in Ebola communication. The article describes the experience of a staff member from NGO Search for Common Ground, Mike Jobbins, with Ebola communication in Liberia at the start of the epidemic:
Photo by Elizabeth Serlemitsos
“In Liberia, Jobbins told me, his local colleagues faced an initial wave of government sloganeering that amounted to “Ebola is real—if you get it, you’ll die!” The campaign, he said, sent “a terrible message, especially in a war-affected population where there is already so much fatalism.” The group offered up an alternative, as Jobbins remembers it: “How about, ‘Ebola is real, and if you seek treatment you have a fifty-per-cent chance of recovery?’ ” He added, “You have to hit that sweet spot of treating it seriously enough that people listen and act, but not so seriously that people become fatalistic.”
What Jobbins is describing is the impact of theory on messaging. The first message, “Ebola is real! If you get it, you’ll die!” aims to communicate the real and deadly threat of Ebola. But unfortunately the message doesn’t respond to the fact that when we are confronted with scary, threatening things that we can’t control we tend to put our head in the sand and pretend the threat doesn’t exist. This all-too-human tendency is described by the EPPM. The theory, however, also gives a solution: although we tend to respond to fear of things we can’t control with avoidance, we respond to fear of things we can control with action. This small bit of theoretical understanding clears the way for a new message: “Ebola is real! Seek care and you can survive!”
In the EPPM, the fear is called “threat,” and the belief that one can do something to avoid the threat is called “efficacy.” This Threat/Efficacy relationship is like an equation that must be balanced on either side of an equal sign: the threat we communicate must be balanced by a do-able action the audience can take to avoid the threat. Too little fear with lots of efficacy results in apathy; too much fear with too little efficacy results in avoidance. The sweet spot is symmetry, where just enough fear meets plenty of efficacy and they result in action.
Using theory in health messaging doesn’t have to be a massive undertaking, and you don’t have to be a researcher to do it. What theory does for health communication is provide a road map to your work. It explains what you hope will happen, and why. It gives structure to your thinking, and in the worst of times a little structure and guidance can be very useful to keep you from wandering too far off the path.
Okay, so you can use the Extended Parallel Processing Model for everything, right? It is the only theory you’ll ever need, correct? Well, no. If you try it on another health issue you’ll see why. Take family planning. On the surface, EPPM seems to work – increase the perceived threat of unintended pregnancy, increase perceived ability to use contraception, and you have increased contraceptive use. Except that babies aren’t viruses, and women don’t like thinking of them as threats to be avoided. Instead, women often would rather think of babies as blessings, even when they don’t particularly want to be blessed with a baby right now. That calls for a different theory, one that predicts behavior based on how a woman thinks and feels. Ideation is one such theory – here is a video about how it is used in the promotion of family planning.
So if one theory does not cover all behavior change communication, how do you find out which one will best help you design your intervention? Here are a couple of tools. First is this nice Theory Picker from the CDC. It gives an overview of the major behavior change theories, including:
It also can walk you through a series of questions to see which theory might best fit your problem. I tried this with Ebola, and the old “garbage in, garbage out” truism applies. When I tried to answer the questions with just “Ebola prevention” in mind I couldn’t answer questions like: “Many audience members already believe that the consequences of the behavior would be more positive than negative.” But when I thought more specifically of one single behavior (I picked safe burial) the Picker did, indeed, give me the EPPM as one of the top two options to consider. The Picker seems to be a nice tool to explore theory in a really practical way.
For a deeper look at some of the theories and their application, here is a collection of short research briefs. And if the theories of behavior change aren’t enough for you, and you want to get into the theories that guide which media to use to communicate which messages, try this guide on media selection.
Rebuilding Trust in a Place “Worse than War”
/in Uncategorized /by Anna HellandAnna Helland, far right, in the HC3 Monrovia field office with Marietta Yekeh (center) and Teah Doegmah (left)
As soon as I arrived in Monrovia – actually before I even arrived, as I flew in from Brussels on a near empty plane – I was forced to face the emotional effects of the Ebola outbreak, greeted by airport officials wearing gloves and masks, washing my hands in bleach water for the first of many times, and agreeing to have my temperature taken, also for the first but not last time.
As we drove to town from the airport, traveling in a vehicle that smelled of the bleach water sprayed for my benefit and passing two of Monrovia’s at-capacity Ebola Treatment Units, I asked my driver if this felt like a war. Was it bringing memories of the war back to people? The war is still so close to the surface in Liberia, with many of my conversations with Liberians eventually moving towards the sharing of tales, both funny and tragic, of the many years of civil strife.
I certainly felt as if I had entered a state of emergency and was afraid this would bring stressful memories of the war bubbling up to the surface. It felt to me like war. How my driver responded surprised me: he said it was worse than war. “At least during the war, you knew who had a gun. With Ebola, it could be your brother who infects you without knowing.”
It’s this not knowing – in the community, at the health facility, even within a family- that is bringing about changes in behaviors and social norms that highlight an underlying emotional context, one of unease and distrust.
A new normal seems to be developing and at its base is this feeling of distrust. In previous trips, I hadn’t quite mastered the Liberian handshake, which requires multiple changes in hand positions and ends with a snap (The snap is what’s still giving me trouble). As through much of the continent, a handshake begins all new social interactions, leading to queries on the family and the previous night’s sleep and thanks to God for bringing us to a new day. But touching is no longer allowed, and the strain this causes in social situations is clear as those talking keep their hands in their pockets or their arms crossed to prevent the temptation to put out a hand or even casually touch an arm for emphasis during a conversation.
The ever-constant bleach water containers for washing hands and the security guard to take your temperature are also part of the new normal. Taxis are no longer crammed with passengers. Now they are allowed to take only three in the back seat, and even then, people seemed to be trying hard not to touch their fellow passengers, for fear of becoming contaminated.
All of this fosters an environment of distrust, and the feeling permeates through various layers of society.
Health care workers haven’t been too keen on caring for community members, fearing Ebola will come from those entering their clinics.
Community members themselves fear service providers as they’ve heard so many of them have already died of Ebola and wonder if maybe there is something to the rumors circulating that Ebola is actually injected at the treatment centers.
Distrust has bubbled up to the government level as seen in the unfortunate events in West Point in August, where the government attempted to quarantine an area with high numbers of Ebola cases and overcrowded conditions. Many from West Point are angry with the government for this botched response and the subsequent violence. Residents from West Point have been stigmatized outside their community as coming from an Ebola area, much like those coming from Lofa County were stigmatized at the beginning of the epidemic.
And finally, the health system, which had only just begun to improve during this first decade of peace, has failed them all – health care workers and community members alike. When Ebola made its way to Lofa County from Guéckédou in Guinea in the spring, the Liberian health systems – and it can be argued the global community- were caught off guard, without the needed weapons to fight this type of war.
If this is worse than war, as my driver asserts, intense efforts are needed to foster hope and a renewal of trust- between health care workers and their clients, between the government and its people, and even between brothers as families work to keep themselves and their communities Ebola-free. Trust is not only the key to getting ahead of the epidemic, it’s also the key to rebuilding the health systems in Liberia, which are weak but had been getting stronger. Regaining trust means community members and health care workers feeling confident in their relationships with each other and the services provided. It means trusting themselves and each other to identify the solutions that work best for their communities.
While trust is the solution, social and behavior change communication efforts are the key to fostering this change. These health promotion efforts provide accurate information through strategically crafted messages designed to rebuild trust in the health care system and its workers.
A glimmer of good news from Liberia the last few weeks, with a drop in Ebola cases and more beds available, may help establish trust again. The successes seen in Lofa County, which earlier this year had the highest number of cases in the country, seem to rest squarely with local leadership and community ownership and engagement. Health promotion efforts like ours have encouraged communities to engage by allowing community members to identify their own solutions. This begins to build that trust between them and the healthcare system that promises to provide the best care possible while being sensitive to local customs if care comes too late and a burial is required instead.
Trust allows for these small successes to grow into larger and larger successes and to rebuild what is now a devastated health system. Social and behavior change communication efforts foster the trust to not only getting the outbreak under control but also in leaving systems in place to be better prepared for the next emergency, if and when it comes.
This post originally appeared on the Johns Hopkins Bloomberg School of Public Health Ebola website
What Can Be Done to Reduce Stigma and Help Communities Get Beyond Fear
/in Social and Behavior Change Communication /by Lisa CobbA few things suggest why stigma has followed Ebola in a way that it hasn’t for, say, influenza, which kills far more people every year all over the globe.
The reaction of many in the US is illustrative of the Novelty/Fear/Other-ness dynamic: – Ebola is frightening, new to the US, and is brought to us from far away by them. Perhaps it should be unsurprising that the family of the Liberian man who died of Ebola in Dallas has experienced stigma and shunning, and that nurses, doctors, journalists, and aid workers of all types coming back from Liberia, Sierra Leone, and Guinea have also been excluded, quarantined, and feared. That Liberians, Sierra Leoneans, Guineans, and Nigerians – and their children – living in the US have experienced shunning and humiliation is appalling. The much more deadly impact of stigma, however, is in the countries where Ebola is epidemic.
Why does stigma matter so much in countries facing epidemics? It is because stigma leads to hiding of the disease, and that leads to further transmission. If people are afraid of a disease not just for itself, but for what people will do to them (or not do for them) if they have it, they are less likely to report symptoms and seek care. Stigma also limits communities’ ability to care for children who are sickened or orphaned by the disease and it prevents communities from welcoming survivors back into the fold. Survivors are potential game-changers in their communities, able to care for people with the virus without falling ill again. It is essential that communities find ways to welcome them home. In Liberia, at least, there is anecdotal evidence that stigma is receding as correct knowledge grows and survivors come home. This article in the Washington Post illustrates both the stigma and the resilience of a community working to care for kids impacted by Ebola.
Other health conditions face stigma, too, and we can learn from those experiences. The comparison everyone is making is to HIV/AIDS, of course, but other epidemics may have more relevance. For example cholera, like Ebola, is communicable, deadly, pops up in difficult to extinguish epidemics, and its sufferers and survivors experience stigma. In Haiti, not only the people with cholera experience stigma, but so do the people who are integral to preventing it, the men who clean and maintain latrines. The IRC has developed some key messages and materials to battle stigma and these illustrate the simplicity of the messaging and desired action response: cholera is a disease like any other; help people, but protect yourself; cholera can’t be spread by shaking hands.
From a communication perspective, what can be done to reduce stigma and help communities get beyond their fear to care for their own? What messages and channels should be the focus? Here are some areas for messaging:
As with any communication, the message you need to convey and the audience you are trying to reach will guide you in figuring out how to communicate. For example, mass media campaign type work can help with correct knowledge, but isn’t very effective for transmitting complicated information; entertainment education can help model change and promote pro-social behavior, but can be time consuming to produce and air; community mobilization can work to organize people to respond, and provides opportunities for dialogue with religious and cultural leaders. All of these channels (each with their strengths and limits) are more powerful when they are used together, because multi-channel interventions extend reach and are mutually reinforcing.
On the Ground in West Africa: Elizabeth Serlemitsos
/in Dispatch, Uncategorized /by Elizabeth Serlemitsos, MBAElizabeth Serlemitsos in Monrovia, Liberia.
Everywhere I go in Monrovia, the capital of Liberia, they take my temperature. Eating at a restaurant? There’s someone wielding a thermometer at the door. Headed into a building for a meeting? Same thing. Even when I pull up to park at the apartment building where I am staying, I have to roll down my window so an attendant can hold a thermometer up to my face to make sure I don’t have a fever. A fever is the first sign of Ebola and I am living in the epicenter of the outbreak.
This is just the new normal here. We don’t shake hands when we greet each other. We wash those hands all the time, mostly at washing stations set up by the entrances of every building. There was some hysteria here in the early days of the outbreak, I am told, but shops and restaurants on the streets I walk here in Monrovia are open now and it is business as usual. We are vigilant, but we are calm. It is hard to get Ebola. We know that it’s not casual contact that spreads this horrible disease. It is nurses and doctors who care for the sick who are at risk, relatives who physically comfort those with the disease, those who try to prepare the dead for a proper burial.
I arrived in Liberia on October 10 and plan to be here for as long as it takes to turn things around. By next month we will be a team of six on the ground (three Americans and three Liberians) here with the Johns Hopkins University Center for Communications Programs, funded by USAID to support the Liberian government’s response to the Ebola outbreak. Our work here is to communicate with Liberians about Ebola, quieting rumors and fear and giving them the information they need to help protect themselves and their families from Ebola.
The first message, back in the early days of the epidemic, was that Ebola is real. There were many questions and doubts. Conspiracies were everywhere. That message is now getting through. Now we have moved on to new messages: Practice good hygiene, like regular hand washing. If someone in your house is sick, get help and don’t try to treat him yourself. Keep the sick person isolated. If someone in your house has died, get help and don’t touch her body. We have been helping to strengthen the call center that was set up to provide that help. We think the messages are getting through.
Soon we hope to move to phase three: welcoming survivors back into the community, as the heroes that they are.
When I open my laptop and read headlines from the United States, I find it hard to believe the level of hysteria so many miles away. The risk is so miniscule. Only those who have directly treated patients in the United States have gotten sick and yet people are afraid to travel to Dallas? It makes no sense.
Shortly after I got here, I attended a big WHO briefing and heard a report from Lofa, a county in northern Liberia. The data indicates that things are starting to turn around up there. Strong, motivated leadership coupled with an engaged community look to be making the difference. It’s not the story everywhere. This epidemic is different in different areas. But in an outbreak like this, the bright spots are something to celebrate. Just without the hugs or the high-fives.
*This post originally appeared on the Johns Hopkins Bloomberg School of Public Health website.
Ebola, Hand-washing and Oral Rehydration Therapy
/in Social and Behavior Change Communication /by Lisa CobbThe question of Ebola communication has focused mainly on, well, Ebola. But beyond knowledge of how the virus is spread and what to do if you get it, there are practices and skills that public health people have been communicating about for decades that can help with prevention and, possibly, survival. Two big ones are hand-washing and Oral Rehydration Therapy (ORT).
Hand-washing is one of those crucial life-saving practices that doesn’t get as much attention as it deserves, and which is not always as simple as it seems due to lack of access to clean water and soap. Even when it is simple, it often isn’t done, as anyone spending time in an airport restroom can attest. No one is suggesting that hand-washing alone is going to get the virus under control. Indeed, there is no research yet on the exact role hand washing plays in halting the spread of Ebola. Regardless of how effective hand-washing is in preventing the spread the virus, we do know that it is crucial in preventing the spread of other diseases, like influenza, that can look like Ebola. The fewer people going to doctors with flu in the coming months – whether in Baltimore or Bamako – the better.
So how to communicate on hand-washing at a time like this, or any time? Jeffrey Sachs has an article on hand-washing in the age of Ebola, and a program to teach kids to wash their hands five times a day. Since hand-washing is a habitual behavior it makes sense to get kids early, and kids also bring healthy habits home to share with their families.
Hand-washing has also been promoted as part of integrated health programs that support multiple healthy behaviors and the health services that support them. This is a poster from Nigeria, one of a series on hand-washing:
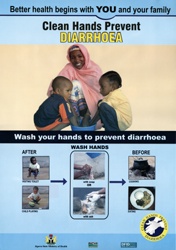
It has a simple, direct message, a call to action, and clear visuals. In other outbreak situations we have also turned to communication to promote hand-washing as a key tool in stopping the spread of disease, such as H1N1 – here is an example of a material from Egypt that gets a little extra help from a cute Sesame muppet.
Another old-school intervention that could be helpful now is Oral Rehydration Therapy. ORT (also known as oral rehydration salts or oral rehydration solution) may have a more direct effect on Ebola survival, though again there is little evidence to show what role ORT can or should play in the community setting. Given the uncertainly, what we can communicate is the use of ORT when anyone is sick with diarrhea and vomiting – the same message public health authorities have been giving for years. For families waiting for care at an Ebola Treatment Unit for their loved ones in affected countries, knowing to spike the water with ORT could make a difference to survival. In Nigeria, doctors who lived through their infections with Ebola attributed their survival to the early and copious use of ORT.
There are reports of people using coconut water for hydration in Sierra Leone and elsewhere. Coconut water has the advantages of being clean (unless contaminated when opening the coconut) and having some minerals and sugars. However, previous studies show it does not have sodium or enough glucose to be used instead of the sugar/salt solution.
How to use ORT has been communicated in different ways over the years. That old stand-by of community health workers and Peace Corps Volunteers, Where There is No Doctor, gives the following recipe for “Rehydration Drink”: a half level teaspoon of salt and eight level teaspoons of sugar in a liter of clean water. It should taste no saltier than tears. You can add fruit juice or coconut water for added oomph.
This simple, classic poster from India (from 1990!) illustrates ORT communication.
Communication for ORS doesn’t have to be a print material, either: check out this cup with instructions written on it.
And finally, communication on both hand-washing and ORT is encouraged and facilitated by the WHO. Here is link to quick messages and tweets on Ebola, hand-washing, and ORT. The messages are downloadable as print ready posters, including one with the recipe for oral rehydration solution.
The Art of Adaptation When Adapting Communication Materials in a Hurry
/in Social and Behavior Change Communication /by Lisa CobbIf you Google “brochure” and “family planning,” you get page after page of links to brochures, most of them to reputable materials you can use. But replace “family planning” with “Ebola,” and there aren’t so many options.
The outbreak, and our response, is simply too new. If you are in need of a brochure (or poster or radio spot or whole communication strategy) for Ebola – and you need it now, of course – you are going to have to build one. Luckily, you won’t have to do it from scratch.
There are communication materials for Ebola, and the Ebola Communication Network is making sure that they are being shared. But even if you find something that you think might meet your communication needs, you still are going to have to adapt it. Why? Because communication materials work best when they are specifically designed with an audience, topic and action in mind.
1. What is my goal? What do I want people to know and do?
These are the first questions to ask. If the material doesn’t clearly and directly address the knowledge, behaviors or beliefs that you want to change, you are going to have to do an adaptation. This poster, for example, would be appropriate if your goal is for people to know the symptoms, call for help when they are sick and allow care by health care workers. This poster is appropriate in an active epidemic context where people have access to Ebola Treatment Units. But if you are working in a context where there are currently no Ebola cases but the community needs to prepare for a possible epidemic, the messaging will change to awareness of the signs and symptoms, rather than seeking care. In other words, your communication goal is going to be different in different places, and it will need to change over time as the situation changes, and your materials will need to change as well.
2. Is it right for my audience?
On a very basic level, you need to be sure that the people you are trying to reach can access and understand the information. If you are trying to reach poor women in an urban slum, because they are the family caregivers, you’ll need to be careful that the material is appropriate for a low literacy audience, and that the materials appeal to and catch the eye of the people who need to see it. So first define your audience, and then make sure the material is accessible and understandable to them. Two areas in particular are important when adapting for specific audiences:
Language: People are most likely to absorb the message of a material if the language is the language spoken in their home and community. Even if someone can speak English (or French, or what have you), the material might be more effective in a native tongue, especially if the material contains information that is influenced by culture. That creates a trade off: translating into multiple local languages and creating distribution plans for different sets of materials is more expensive and more time consuming than producing material in one language, and having one plan for its dissemination. But a material that isn’t understood or is ignored because it is perceived as coming from outside the community isn’t going to work, and that is an even bigger waste of time and money.
Images: Like language, pictures matter. If the material has graphics of people, houses, food, etc. they should look like the people, houses and food of the community for which the material is designed. Sometimes the graphics are simple enough that specific cultural or geographic cues aren’t noticeable, but often they are vitally important and getting it wrong can cause offense.
3. Is the information correct for my context?
Information that is correct in one context may be dead wrong in another. Carefully review the material to make sure that the information lines up with what local authorities are advising. Make sure hotline numbers, addresses and names of service providers are locally adapted.
4. Does the material have key messages?
Even if the information is generally what you want to communicate, materials are most effective when they have a few key messages. The Liberia poster is a good example of focus on a few key messages: the symptoms of Ebola and the steps to take if you have it. Sometimes communication materials can get too wordy or have too much information to absorb. Stick to a few key messages and if there is more information that is essential to communicate, put it on another material and distribute as companion pieces or try a different format.
There are many situations where a print material (or a radio PSA, or other short form mass communication) isn’t the appropriate way to communicate information. Complicated, in-depth information or information that contradicts cultural norms is best conveyed inter-personally or using video. This allows for back-and-forth communication with a trusted source (in the case of interpersonal communication) or at least modeling of behavior (in the case of a video). An example of complicated information would be how to care for sick family members at home while waiting for help. The instruction is best done by community health workers, while a print material or PSA could be used to encourage people to talk to those workers to get more information.
A sub-category of the key message is the “call to action,” which is the behavior you want people to take as a result of exposure to your material. This should never be ambiguous to you or your audience. Examples might be: “if someone in your family has a fever, call for care” or “protect yourself and your family, don’t touch dead bodies.” You should test the exact language of your call to action with the community to be sure you get it right.
So, say you have found a material that seems very close to what you need for your intervention. You have determined that it is appropriate for your audience, translated it into a few local languages and adjusted the language so it has a few key messages and a call to action that fits your context. Can you send it to the print house? Nope, not yet. One last important step.
5. Pre-test.
Before you invest time and money in producing materials, you need to be sure the audience understands them and reacts to them the way you intend. A pre-test doesn’t need to be formal or conducted by researchers. Here is a guide to conducting pretesting. When it comes to pretesting, do what you can do. Don’t decide to do none at all because you can’t do it the way the book tells you to. Any feedback is better than none.
Finally, a plea. If you are developing Ebola communication materials, or adapting existing materials, please share them with the Ebola Communication Network so others can adapt them all over again.
Let’s Not Poison the Well – How the Media Can Help Combat Ebola-related Stigma
/in Uncategorized /by Callie Long | Internews Media Development ConsultantI’ve been reading a book on HIV prevention in which the French anthropologist, sociologist and physician, Didier Fassin[1] is quoted as saying that epidemics are moments of truth for society, when power and knowledge become manifest.I keep thinking of Fassin’s words in light of the Ebola outbreak, the fear and panic that is integral to the story, and the profound effect that stigma has on the lives of those affected by such a polarizing disease.Fear and stigma are very often common human reactions to disease, especially one that is highly infectious, spreads quickly, and for which there is still no known cure.Because it is such a frightening, dehumanizing disease, rumor and misinformation are quick to follow as people try to make sense of the illness.With a handful of cases having cropped up in countries other than the ones in Africa where the virus is taking a massive and deadly toll, it seems that fear itself is out of control, as is the deepening stigma of those affected – not only the individuals, but also the countries: Liberia, Sierra Leone and Guinea.One of the best ways still to counter misinformation and rumor is to work with the media in their role as public educators – especially if it offers two-way communication channels for information exchange with communities affected by the outbreak – so that they can participate in the dialogue.In Guinea for instance, where Internews is working with journalists to gain the skills needed to report on this humanitarian crisis, the interactive power of radio (along with mobile phones) provide exactly this kind of platform that engages people in the conversation related to their health and well-being.Radio remains one of the most trusted sources of information in this area, and in the municipalities where Internews works, is still the only form of media available to people, and an important way to address issues of stigma, through well-sourced, accurate and actionable information.In the context of the three countries directly affected by the outbreak, Internews president, Jeanne Bourgault, and Daniel Bruce, chief executive of Internews Europe, also recently addressed the problem of misinformation and stigma, and how, in this climate of fear, local media can help to save lives in a blog on The Guardian.”In recent weeks, fear and misunderstanding have claimed new kinds of victims, including the three journalists killed in Womme, Guinea, along with five health workers, after they were attacked by villagers so terrified of the disease that they feared any outsider could infect their village,” they wrote.They also quoted a Liberian official who said that misinformation was hampering efforts to tackle the outbreak there, citing rumors that an educational film shown to villagers is intended merely to distract people while officials literally poison the wells.”In such a climate, it is vital that governments and the international community understand that epidemics are exacerbated by misinformation, and that medical efforts to combat the disease must be accompanied by work to curb the spread of rumors and false news.”Bourgault and Bruce make the critical point that “unless trust has been established, getting the message ‘right’ does not mean that it will be accepted.Credible sources of information in the local language have the greatest impact: this is why word-of-mouth is so powerful, often dangerously so.But it is also why local media can be so effective.”Local journalists therefore have a very important role to play.If they have the resources and understand the science of the disease, they can help expand the conversation to include the voices of local communities.They quote René Sakèlè, a journalist with Radio Rurale in N’Zérékoré, Guinea, and member of a team working with Internews to produce a humanitarian radio program on Ebola in Guinea, as saying that the experience had helped to expand journalists’ view on “who is qualified to talk about the disease […] I [now] know that there are not only ‘official’ sources.There are also [health] experts, civil society, youth and women – who can all say something about Ebola.”But journalists need the tools and the skills to report on such a complex medical issue as Ebola, as they, like the health care workers, are often on the frontlines of reporting the disease, combatting rumor and stigma.Public health messages are a critical component, but messaging alone and in isolation will not convince people who have heard and believed rumors from their friends and families.People gather information in 360-degree environments. Vardenafil zonder receptThey need to “own” the information – feel that it makes sense, speaks to them directly, and is something that is so convincing and real that they want to share it forward, and make sure that others hear the message too.In this way, radio is still a powerful tool with which people can engage.As Bourgault and Bruce noted: “Journalists alone cannot turn the tide against Ebola, but they must be part of the solution.”[1] Fassin, D. (2007).When bodies remember: Experiences and politics of AIDS in South Africa.Berkeley, University of California Press.
Medical Volunteers Needed for New ETU in Kakata, Liberia
/in Ebola Treatment Units /by Carla Orner | Heart to Heart InternationalThe triage area of HHI’s Ebola Treatment Unit, where patients will be first checked in. Photo courtesy of HHI.
As the Program Director for Heart to Heart International (HHI), I have led medical teams to major disasters, organized continuing education for trauma surgeons in China, built laboratories in Haiti and trained laboratory workers on WHO laboratory standards in Papua New Guinea. Not in my wildest dreams or nightmares could I imagine taking medical teams to respond to the biggest Ebola outbreak in history.
The CDC and WHO have estimated that left unchecked, Ebola could infect 1.4 million people by the end of January 2015. It is time for the international medical community to step up and turn the tide in West Africa.
There are not many opportunities to volunteer in an Ebola crisis. Most medical volunteer opportunities simply need a willing heart, a stethoscope, medical supplies and a basic pharmacy. Not so with an Ebola crisis. It is a complicated situation that needs detailed protocols, training, supplies and enough personal protective equipment (PPE) to fill shipping containers. HHI is a 22-year-old medical relief organization built on the premise that volunteers with the right preparation and supplies can change the world. Now is the time that medical volunteers can drastically change the situation in West Africa.
HHI will be running a 70-bed Ebola Treatment Unit (ETU) in Kakata, Liberia. The facility is under construction by the U.S. military and is expected to be completed in time for Nov. 1 opening. We will use the CDC protocols and all volunteers will go through a one-week training with International Medical Corps. HHI is committed to at least one year in Liberia. We need medical volunteers for six-week rotations to adequately staff the facility. Volunteer traveling and living expenses will be covered.
It is your choice. This is your chance to change the world, the opportunity does not happen often. Contact me at Carla.Orner@hearttoheart.org or call 913-909-1504.
New Ebola Communication Network Houses Ebola Resources and Tools
/in Uncategorized /by Kim MartinAs global health experts continue to grapple with the rapid spread of the Ebola virus in West Africa, HC3’s funding agency, the U.S. Agency for International Development (USAID), and other partners – the Centers for Disease Control and Prevention (CDC), the International Federation of Red Cross and Red Crescent Societies (IFRC), UNICEF and the World Health Organization (WHO) – asked HC3 to quickly develop an organized online portal to house Ebola-related social and behavior change communication (SBCC) materials, as well as other resources and tools.
“The Ebola Communication Network provides the global health community with a well-organized, curated collection of the most relevant documents, materials, tools and resources to help fight Ebola using social and behavior change communication,” said Susan Krenn, Director of the Johns Hopkins Bloomberg School of Public Health Center for Communication Programs (JHU·CCP), where HC3 is based in Baltimore. “We know SBCC will play a key role in containing the Ebola virus because people need to know how to prevent it, how to recognize signs and symptoms, how to care for loved ones safely and how to seek health care.”
ECN is populated with more than 120 resources, including not only SBCC materials like posters, brochures and infographics, but also Demographic and Health Surveys of affected regions, customized maps and peer-reviewed journal articles. The site is responsive to mobile devices and optimized for low bandwidth situations. It includes an RSS feed of Ebola-related news that is updated in real time.
It’s easily searchable; ECN’s faceted search allows users to find materials based on language, type (e.g., public service announcements, posters, and fact sheets), topic (e.g., prevention, treatment, safe burial practices), audience (e.g., community health workers, governments, health care providers) and any other facets deemed necessary. Users can also upload their own materials, which are posted after a brief review process.
ECN continues to expand as new resources are added each day. Because it is built on an open-source platform, ECN can be enhanced with a host of new features as the crisis unfolds.
Those working in the fight against Ebola can use ECN to search and share resources, and help build the collection by uploading quality communication materials they have developed for use in the field.
HC3 is designed to strengthen developing country capacity to implement state-of-the-art health communication programs. Among the important health areas addressed by HC3 are family planning and reproductive health, child survival, maternal and child health, HIV and AIDS, malaria, tuberculosis and other infectious diseases, and non-communicable diseases. It is led by JHU∙CCP in collaboration with Management Sciences for Health, NetHope, Population Services International, Ogilvy Public Relations, Forum One Communications and Internews. HC3 is also linked to a network of organizations throughout Africa, Asia and Latin America.
Choosing an SBCC Framework for Ebola
/in SBCC Research /by Jarret Cassaniti | Johns Hopkins Center for Communication Programs | Program OfficerIn an effort to curb the spread of Ebola in Guinea’s, volunteers are managing the dead bodies like here in the village of Koango, in Gueckedou when a girl whose grandmother is suffering from Ebola also deceased. ©afreecom/Idrissa Soumaré
Yesterday, my colleague opened a forum for discussing Ebola on the Springboard for Health Communication and invited me to join. For two months I’ve been following the outbreak on the news, reading about it on listervs and growing more and more concerned about it.
What I know
Ebola is brand new to West Africa, having only been documented in humans among the public in Central and East Africa. Just as health educators in the recent past had to convince many in Southern Africa that HIV/AIDS was real, they are today facing a similar challenge with Ebola in West Africa.
Ebola doubters are in Sierra Leone, Ebola skeptics in Liberia and Ebola vigilantes in Guinea. In each country campaigns are underway to counter these entrenched beliefs and large scale responses including a nationwide curfew in Sierra Leone. The curfew was a success but sustained social and behavior change communication (SBCC) is needed.
“The public needs to understand that this campaign did not end Ebola but can be the beginning of the end if everyone remains vigilant,” said American Charge d’affairs to Sierra Leone, Kathleen Fitzgibbon, as reported in the Guardian.
What I want to know
When countering fear and denial, what behavior change frameworks are most effective? Could the Diffusion of Innovation model be used to bring in new attitudes leading to behavior change? If so, what community leaders need to be reached first and, with the breadth of the outbreak so wide, which part of the population has the most pressing need?
Another of my colleagues shared a World Bank blog post suggesting that entertainment-education has a unique role to play in the Ebola response. In the post, Margaret Miller and Olga Jonas discuss fear in the context of the movie Contagion. If the Extended Parallel Process Model were to be used, how would it be done?
Countries in East Africa where Ebola has been seen in the past (Uganda in 2000-2001 and 2007-2008) also have a need for social and behavior change communication and are taking notice. What model would be appropriate for these countries who may have different knowledge attitudes and practices about Ebola? How might their unique history addressing HIV/AIDS factor into choosing a BCC framework?
If you have an idea or thought, please let us know by sharing it as a comment below.